The Gut – Brain Connection
Disclosure: We use affiliate links and may receive a small commission on purchases.
 The Gut – Brain Connection
thefitbay.com
The Gut – Brain Connection
thefitbay.com
Have you ever felt that sinking feeling in your gut when you hear some bad news, or feel sick to your stomach before a big presentation? Perhaps you have days where you feel grumpy or sad for no apparent reason, or maybe you’ve been suffering from chronic depression and anxiety that seems to be impervious to all manner of treatments.
As it turns out, that “butterflies in your tummy”, nauseated feeling you get when you are nervous or stressed and depression, anxiety, and mood swings are actually connected on something called the gut-brain axis, and the secret to healing depression and improving your mood lies at the bottom of your belly.
What is the Gut-Brain Connection?
Scientists and researchers are now calling the stomach the “second brain”, or more formally the Enteric Nervous System (ENS). It is a double layer of hundreds of millions of nerve cells that line the walls of your digestive system, all the way from your esophagus (in your throat) to your rectum (where you remove waste). It is through the ENS that the brain is continually sending signals to the stomach, and the stomach is continually sending signals back to the brain, they are constantly in communication. We have known for a while that a primary role of these signals to facilitate digestion and ensure we don’t starve:
- The stomach sends signals to the brain to let us know we’re hungry
- The brain sends signals back to the stomach to release gastric juices to prepare the stomach and intestines for digestion
- The stomach sends signals back to the brain to tell us we’re full and don’t need any more food
All of this is done through a series of hormones, nerves, and neurons. As we are now learning, however, our brain and gut are connected on a much more intimate level.
How the Gut Affects Your Mood

In a chicken-and-the-egg scenario, a troubled brain can cause a distressed gut, and so can a distressed gut cause trouble for our brain. This can cause that queasy feeling before a first date, but can also mean more serious mood disorders like anxiety and depressive episodes. Essentially, irritation in your gastrointestinal tract, such as irritable bowel syndrome, diarrhea, pain, inflammation, bloating, and stomach upset, sends signals to your Central Nervous System (CNS) that cause changes in your mood. Considering that anywhere from 30 to 40 percent of the population suffers from gastrointestinal problems, it’s no wonder that depression and anxiety are on the rise. While acute stress, such as a big presentation at work or school, can cause temporary tummy upset, it’s these chronic gut problems that are of the greatest concern, as they are what is permanently affecting our brain and mood. The question remains, what is causing these issues?
The Microbiome and Your Mood
In your GI tract, you have millions of bacteria that play a huge role in the health of your gut and intestinal lining. Most of this bacteria is good for you and helps you digest food, protect against inflammation and infection, and modulate signals between your ENS and CNS (your gut and brain). As long as you have enough good bacteria and they outnumber any bad bacteria that inevitably come along, you will have a normal, healthy functioning gut and ENS. When the balance is off, however, that’s when gut disorders and mental health issues strike.
What Causes Changes to Your Microbiome?
Stomach bugs, flus, food poisoning, and really anything that causes vomiting, diarrhea, and even constipation can seriously disturb the environment of your intestinal tract. While those will typically ‘right’ themselves after a few days, what causes more issues for your gut are the chronic, everyday stresses we tend to put on it. These are generally in two camps: Drugs and Diet.
The Drugs

A common side effect for most drugs, both prescription and over-the-counter, is stomach problems. The reality is, drugs are just hard on your digestive system in general. Even common medications such as ibuprofen, Aspirin, and Tylenol can do damage to the bacteria in your gut and your intestinal walls. While popping an advil for the occasional headache won’t cause too much distress, many of us use these drugs daily, instead of taking the time and making the lifestyle changes that would actually cure chronic pain. This then becomes cyclical:
- We are in pain, so we take a painkiller.
- Overtime, use of that pain killer severely damages our intestinal lining, causing both more physical pain and increased pain perception by the ENS.
- In response, we take more pain meds and so the cycle continues.
The worst offender for causing an out-of-balance microbiome, however, is our society’s reliance on antibiotics. While antibiotics are important and have saved thousands of lives, they are non-specific, which means they kill of both the good and bad bacteria in our guts. Our chronic use of antibiotics is affecting our gut and our brain in the same way the pain meds are.
Our Diet
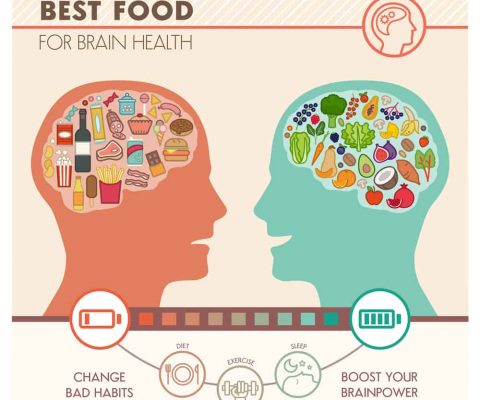
Let’s face it: Our diets and lifestyles leave much to be desired. We spend most of our days sitting, are chronically dehydrated, eat far too much sugar and processed garbage, and even so-called “good for you” foods contain additives, preservatives, and other chemicals that we are ingesting on a regular basis.
Sugar
The bacteria in our bodies feed on sugar. When we eat too much of it, our intestines become overpopulated which overtime causes bloating, indigestion, and other digestive disorders. The more the walls of the ENS become damage, the greater effect this has on the communication between the gut and brain. Distress signals are sent out, and we become anxious, more likely to ‘snap’ or have an emotional breakdown, and become depressed.

A study done on the effect of diets high in saturated fats and sugar on mice confirmed what scientists had been suspicious of:
After 13 weeks, the mice on the high-fat diet showed much less motivation and decreased memory than the control group. The high-sugar diet mice were less goal-oriented and motivated than the control, and both groups showed higher rates of anxiety, along with physical symptoms such as weight gain.
Food Additives and Chemicals
Whether it’s the additives in processed foods (which also happen to be high in fat and sugar!), or it’s the pesticides and insecticides sprayed onto non-organic produce, there’s no doubt that these chemical ingredients are messing with our gut and our mind. Many of these ingredients are approved by the FDA and other governing bodies because they have not shown to cause harm to human cells. While that may be true, there are far more bacterial cells in our digestive tracts than human ones, and as we now know when those are damaged, gut disorders (IBS, Crohn’s, Diarrhea, Constipation, etc) ensue and along with them come mental health problems.
Heal the Gut, Heal the Mind
Now that you have a basic understanding of how the brain and the gut are connected and what happens to the brain when your gut is unhealthy, it’s time to talk healing. These are the steps you should follow to solve your gut problems, lift your mood, and clear your mind:
Cut out sugar and processed foods.
Plain and simple, stop eating these foods. They are not good for you, despite what their packaging might say. Even “whole grain” breads, cereals, granola bars, and other packaged products are high in fat, sugar, additives, and preservatives. If you don’t believe me, read the label! Replace these with homemade sugar free versions and whole foods such as potatoes, sweet potatoes, vegetables, and fruits.
Elimination diet.
Whether we realize it or not, many of us are eating foods every day that are causing distress in our GI tract. Common offenders include:
A. Wheat and grains
B. Dairy
C. Nightshades (Potatoes, Tomatoes, Red Peppers, Eggplant, etc.)
Remove one of these at a time for an entire month and take note of how you look and feel. Changes in your skin, hair, and nails, energy levels, mood, ability to concentrate and focus, bloating, weight, inflammation, and joint pain. While certain foods, such as wheat and dairy, you may find best to avoid regularly, others (nightshades, eggs, other grains) you may find you can add back in once your intestinal lining has healed.
Consume probiotics.

After years of damaging your intestines, you will need to repopulate your intestines with good bacteria. You can do this by taking a probiotic, or by including probiotic rich foods in your diet, such as:
- Kefir
- Kombucha
- Kimchi
- Saurkraut
- Some yogurts
- Other fermented foods (some pickles, sourdough breads)
Be sure to talk to your doctor or visit a naturopathic doctor before taking any new supplements.
Eat more vegetables.
Especially the green ones! Vegetables will provide your body with the anti-inflammatory, antioxidant, vitamins and minerals it needs for health and healing. They are also high in fiber that will help you to effectively eliminate waste and the bad bacteria that has built up in your colon.
Drink plenty of water.
Water is involved in every process in your body, and is crucial for healing and waste elimination. An excellent way to know if you are drinking enough water (which will be different for everyone) is by the color of your urine: If it’s pale yellow, you are doing well, if it is medium to dark yellow, than you need to drink more.
The Bottom Line
Your brain and your gastrointestinal tract are intimately connected, and when one is off, they both will be. Though more research is being done to better understand how the ENS and CNS affect each other, one thing remains clear: Take care of your gut, and your mental health will improve. Taking these steps towards healing will ensure you live a healthy, happy life.